World AIDS Day takes place on December 1st every year, providing an opportunity for people globally to unite in the fight against HIV, show support for people living with HIV, and to commemorate those who died from AIDS-related illness.
World AIDS Day was the 1st global health day, founded in 1988, with the Red Ribbon becoming an internationally recognised symbol of HIV and AIDS awareness; created by the group Visual AIDS in 1991. The red ribbon is worn by people throughout the year in support of people living with HIV and in remembrance of those who have died, but on World AIDS Day the red ribbon highlights the solidarity for people living with HIV and is worn as a simple yet powerful way to challenge stigma and prejudice.
This year there are many campaigns for World AIDS Day 2017 (#WAD2017). In the United States of America, this years theme from the U.S Agency for international Development (USAID) is “Increasing Impact through Transparency, Accountability, and Partnerships”; reflecting on the impact of global partnerships. In the United Kingdom the theme from the British HIV Association (BHIVA) is “HIV: Towards Zero” (#HIVZero) to celebrate the progress and achievements made in HIV diagnosis and management, whilst highlighting the challenges that remain. The South African National AIDS Council (SANAC) has adopted the global UNAIDS theme of “Right to Health” (#myrighttohealth); the right of everyone to the enjoyment of the highest attainable standards of physical and mental health. This includes people living with and affected by HIV, to the prevention and treatment of ill health, to make decisions about ones own health and to be treated with respect and dignity and without discrimination. Almost all of the Sustainable Development Goals are linked in some way to health, so achieving the Sustainable Development Goals (which includes ending the AIDS epidemic) depends on ensuring the “Right to Health”.
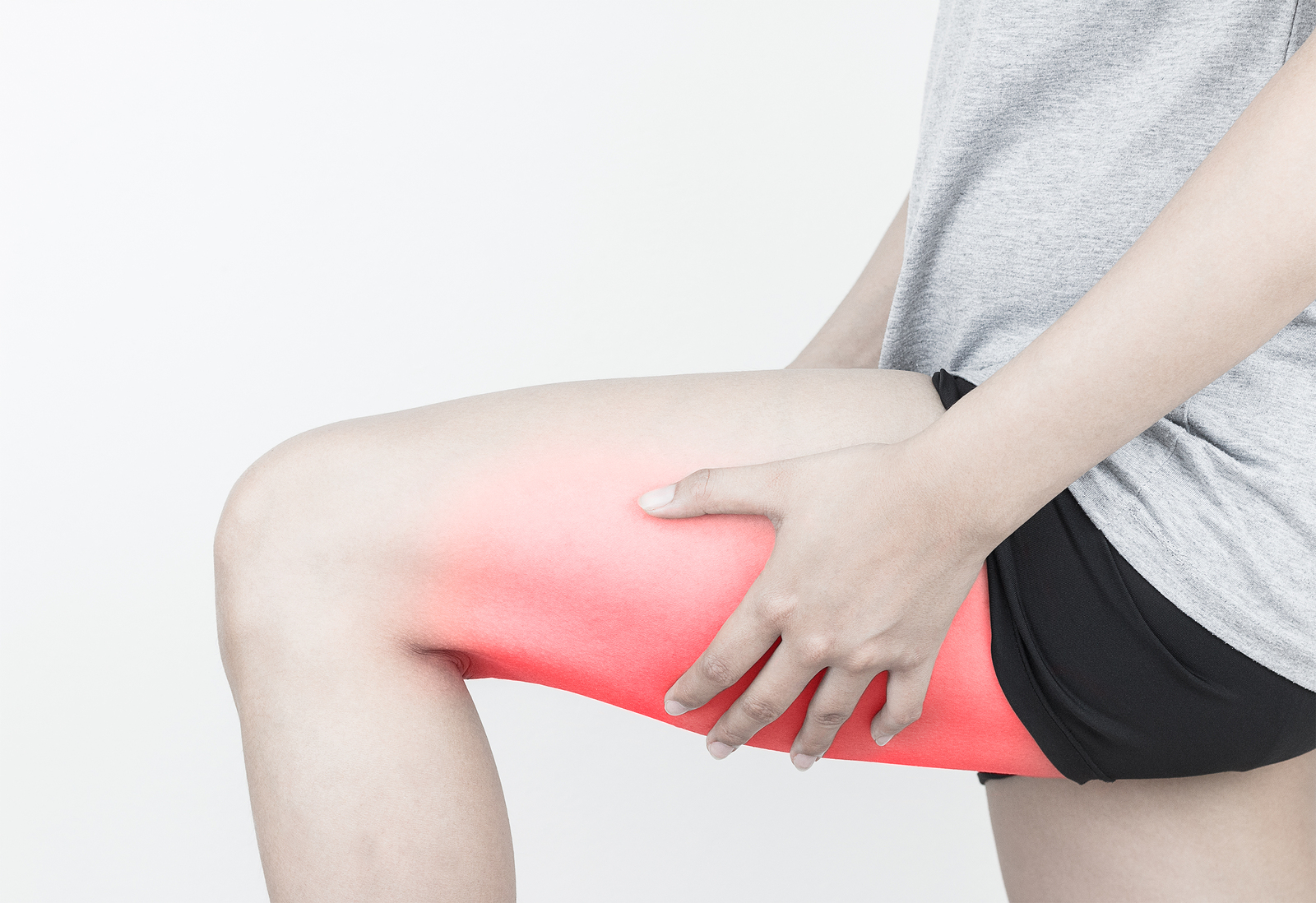
Good health is a prerequisite for progress on ending AIDS. Ensuring healthy lives and promoting well-being for all at all ages, including people living with or at risk of HIV, is essential to sustainable development. In my previous blogs I have spoken about the role that Physiotherapists play in supporting people living with HIV. Increasing service integration in a way that responds to individuals’ needs, can lead the way in reshaping efficient, accessible and equitable health services for HIV and beyond – and this should include Physiotherapy and rehabilitation. The World Health Organisations “Rehabilitation 2030: a call to action” highlights the increasing unmet needs to people with long term health conditions globally, experiencing disability and requiring rehabilitation. So for World AIDS Day 2017, I want to champion the role of Physiotherapists in supporting people living with HIV, to live healthy lives and promote well-being for all at all ages. Physiotherapy and Rehabilitation fits into this year’s theme of “Right to Health”, because it is a right to access Physiotherapy for people living with HIV who experience disability, cannot engage in exercise, are frail or have unmet rehabilitation needs.
World AIDS Day 2017 is a chance to celebrate successes and highlight remaining challenges, but it must also be a time for reflection and remembrance to all those we have lost; as demonstrated in this recent article from the Guardian about the book “The Ward”, which has an exhibition in London until 3rd December. This reflection should allow us to feel proud in how much HIV has changed, how “we live in such different times”, and how we will never forget those we loved, those we cared for, those we lost.
So this World AIDS Day, wear your red ribbon with pride, passion, solidarity, support, anger, love, compassion, in memory, or in any way you that feel right for you.